Finding explains failure of drugs that target host vasculature.
Alla Katsnelson
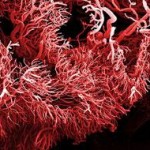
Tumours don’t just rely on their host’s blood vessels for nourishment — they can make their own vasculature, according to two independent studies from the United States and Italy. The findings offer an explanation for why a class of drug once heralded as a game-changer in cancer treatment is proving less effective than had been hoped.
Almost four decades ago, Judah Folkman, a cell biologist at Harvard Medical School in Boston, Massachusetts, proposed that tumours were dependent on the blood vessels surrounding them, and that choking off that blood supply would kill the cancer1. Bevacizumab (Avastin), the first drug to block blood-vessel growth, was approved in 2004, but it and other ‘angiogenesis inhibitors’ have proved disappointing in the clinic, extending patients’ lives for at best a few months.
Now two studies published online today in Nature have identified blood vessels grown directly from cancer cells. So Avastin and drugs like it may be targeting a pathway that is not present in those tumour-made vessels, says David Cheresh, a cancer biologist at the University of California, San Diego, who was not involved in either study. When it comes to treatment, “most people agree that a single pathway is not going to do it,” he says.
Telltale markers
In both studies, researchers worked with tumour samples from patients with an aggressive type of brain cancer called glioblastoma. They found that many of the blood-vessel cells within the tumours contained genetic markers characteristic of the cancer cells, suggesting that the blood vessels were of tumour origin.
The researchers then used markers to identify a subset of tumour cells known to have stem-cell-like properties — that is, the ability to develop into cells with different functions. In a dish, these cells could make blood vessels and, when they were injected into the brains of mice, tumours developed with blood vessels that clearly came from the original human cells. Those stem-like cells, the researchers concluded, could form both tumour and blood vessel.
Such cells seemed to be first making blood-vessel precursor cells, and then differentiating into blood-vessel cells. One of the groups, led by Viviane Tabar, a neurosurgeon and stem-cell researcher at the Memorial Sloan-Kettering Cancer Center in New York City, applied Avastin to cells in a dish to try to block these events. Although the drug did affect differentiation into blood-vessel cells, “we found that Avastin does not alter that first process whatsoever,” says Tabar.
In the second study, Ruggero De Maria from the Italian National Institute of Health in Rome and his colleagues selectively killed the tumour-related blood-vessel cells. This caused the tumours to shrink, showing their reliance on those blood vessels. However, the number of tumour-derived blood-vessel cells in each tumour sample varied from 20% to 90%, suggesting that blood-vessel formation was more important for some tumour cells than others.
Tabar says that it is not clear whether this self-vascularizing capacity is widely present in other tumour types, although there are some hints that this is the case. “It would be very exciting if other tumour cells exhibit the same phenomenon,” she says.
Two-pronged attack
This isn’t the first time researchers have suggested that cancer cells can make their own blood vessels. In 1999, Mary Hendrix, a cancer researcher now at Northwestern University in Chicago, Illinois, and her colleagues reported a similar effect in melanoma cells which they called “vascular mimicry”4.
At the time, says Hendrix, her group predicted that these vascular cells would prevent drugs such as Avastin from being fully effective, but their findings were controversial. The two latest studies support the idea’s validity, she says, as well as demonstrating “an example of the functional plasticity of tumour cells”.
Such plasticity means that researchers must look for a combination therapy that can target both the host vasculature, as Avastin does, and the stem-like cancer cells that can create both vasculature and tumour tissue, Hendrix adds.
Cheresh agrees. Today’s findings in glioblastoma are not the only recent strike against anti-angiogenesis drugs. In the last two years, a handful of studies have reported that, counterintuitively, such drugs can speed tumour growth (see Cutting off cancer’s supply lines, 2009)5,6,7,8. But that doesn’t mean that the strategy of targeting the blood supply is inherently faulty, says Cheresh, who co-authored two such studies.
“There are many more ways to affect the vasculature” than through such drugs, he notes: “It means we need to identify either more than one drug” to shut down blood vessels of tumour and non-tumour origin, “or a common molecular mechanism affecting both the tumour and the vasculature”.
References
- Folkman, J. N. Engl. J. Med. 285, 1182-1186 (1971).
- Wang, R. et al. Nature advance online publication doi:10.1038/nature09624 (2010).
- Ricci-Vitiani, L. et al. Nature advance online publication doi:10.1038/nature09557 (2010).
- Maniotis, E. J.[/author] et al. Am J. Pathol 155, 739-752 1999.
- Pàez-Ribes, M. et al. Cancer Cell 15, 220-231 (2009).
- Ebos, J. M. L. et al. Cancer Cell 15, 232-239 (2009).
- Greenberg, J. I. et al. Nature 456, 809-813 (2008).
- Stockmann, C. et al. Nature 456, 814-818 (2008).